Changes to the CQC Regulatory Framework: What We Know So Far
As the pilot scheme for the CQC’s new regulatory framework gets underway, we look at the roadmap for the changes and what to expect.
Earlier this year, the Care Quality Commission (CQC) announced major changes to the framework it uses to regulates health and social care providers.
Some earlier changes were made to contend with the pressures of the pandemic, such as reviewing how physical, onsite inspections are carried out moving forward, while others, are new.
The new framework forms part of a wider public sector effort to embrace and harness data, and there will also be a renewed focus on sustainability, staff wellbeing and equality.
What changes are planned?
A new way of inspecting
Previously, the CQC assessed care services solely through onsite inspection, gathering all the evidence through visits alone. Under the new model, the commission is moving to a broader, continuous approach by collecting evidence on an ongoing basis.
Routine inspections will remain a key element, but other methods will be important too, including submissions from providers and conversations with managers as well as:
- people’s experiences
- feedback from staff and leaders
- observations of care
- feedback from partners
- processes
- outcomes of care
It’s important to note that the CQC will now be able to update a service’s rating at any time without onsite inspection in order to better respond to risk. It also aims to use data more effectively via a range of audit tools in order to simplify the process, tailoring its assessment to different services and to have one framework.
The frequency of care inspections was previously based on a provider’s most recent rating (with some ongoing monitoring), meaning that providers felt it was difficult to improve their rating.
The new continuous approach increases flexibility and frequency, enabling commissioners and stakeholders to be presented with a more accurate assessment quality of care provided. Reports will also be shorter and score-based, making outcomes easier to digest.
A single assessment framework
One of the most important changes is the CQC’s move to a single assessment framework – a strategy that was first introduced in 2021 with the aim of putting the emphasis on care integration, people’s experiences, cultures of safety and learning. Previously, there were different frameworks for the type of service being administered – e.g., hospital care vs adult social care – and for registration and inspection.
The main change with the single framework is to move away from the CQC’s Key Lines of Enquiry (KLOE) to quality statements which providers will now be measured against. This is intended to remove duplication and complexity by setting out one set of overall expectations that apply universally.
The assessment pyramid
To help understand the new single assessment framework, the CQC has illustrated it using a pyramid, which reduces 300 lines of enquiry down to 34 quality statements.
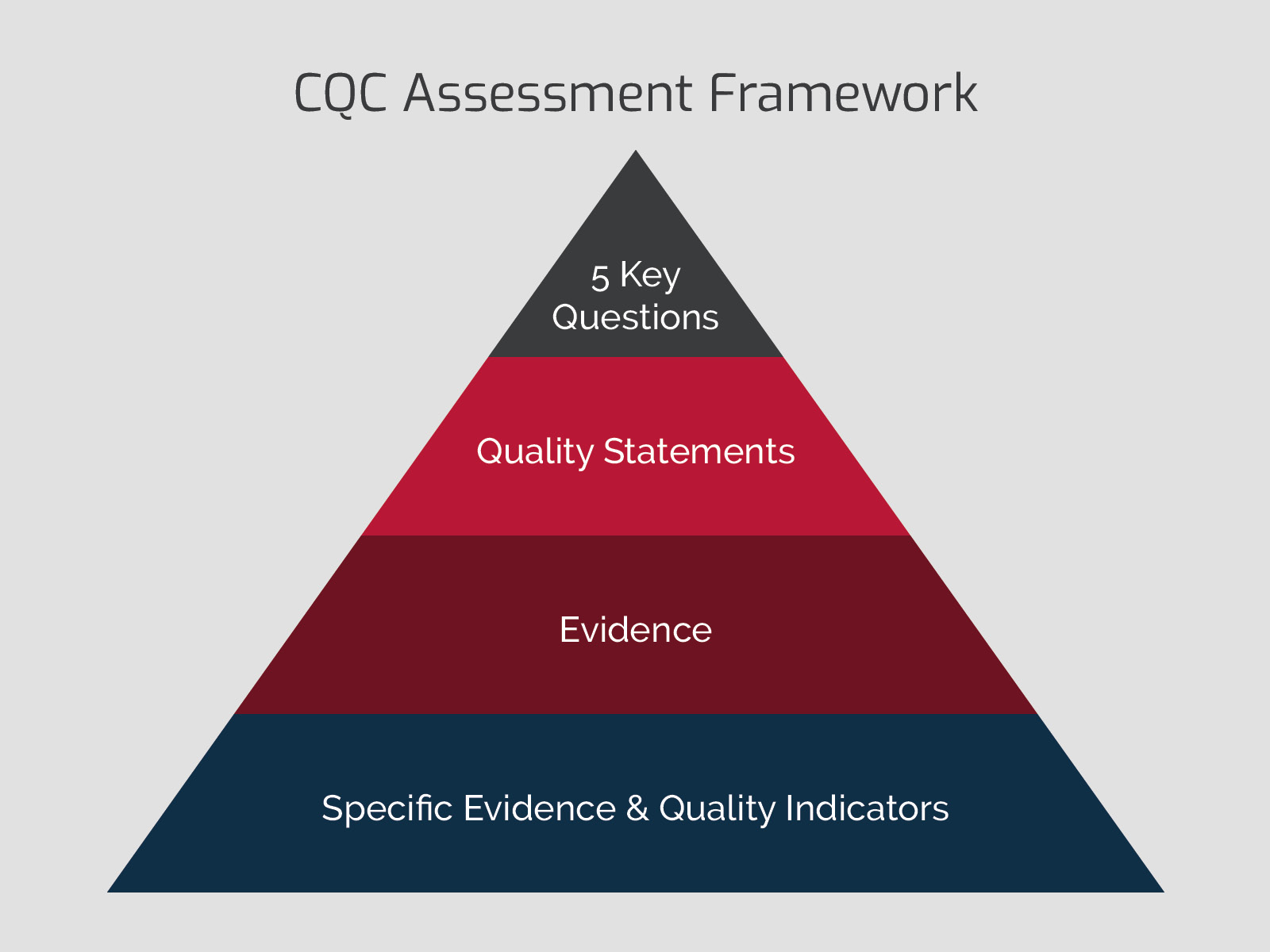
Moving down in chronological order, the top of the pyramid focuses on the ‘five key questions’, which ask whether a care service is safe; effective; caring; responsible; and well-led – these are the same as before.
The next step down is quality statements, which are also known as ‘we statements’. These are examples of behaviours and actions that reflect the five key questions at the top of the pyramid. They’re designed to keep the focus on ‘high-quality, person-centred care.’
The bottom two levels of the pyramid refer to the evidence-gathering stage, with the latter stage more bespoke and specific.
Faster turnaround times
The CQC also hopes that the streamlining of its inspection process should also improve waiting times for results – something that has caused concern in the past. Waiting times have also caused issues for providers hoping to improve their gradings – impacting their status with commissioners and stakeholders.
What’s the timeline for the changes?
The change in approach was first announced in March, along with a timeline for the rollout.
From August, the CQC began rolling out various elements of the new framework to a select group of early adopters. The first group to be invited comprised home carers who had not yet engaged with the CQC’s registration process. They were invited to apply using the new registration portal.
In September, the number of early adopters was expanded to include some GP practices, independent providers, and care homes.
In October, the CQC began carrying out its first assessments using its new approach, again with a small group of early adopters and new services registering.
By the end of 2022, the early adopter pilot schemes will close, and the CQC will report its learnings early in the new year. The commission is aiming for a full rollout in 2023, when it plans to begin assessing all providers using the single assessment framework.
The CQC is taking an iterative approach to these changes, and we don’t yet have all the details, leaving some providers unsure about how best to prepare. At MCP we’re already supporting clients with preparation, and we’ll be providing guidance on the new process every step of the way.
About the author

Carolyn Baker-Mellor is a respected industry leader with over 35 years' experience within the care insurance sector. She works across a wide spectrum of insurance product and policy development, delivery and optimisation for care industry clients, including managing global corporate accounts, working closely with trade associations, and helping clients in protecting their businesses and personal assets.
Care insurance from Towergate
Towergate Insurance are partners with Care England, NCF, Homecare Association and a number of regional associations and are actively engaging with local Government officers to provide updates on market restrictions. We also offer to speak with the CQC oversight committee about challenges within the insurance sector and work closely with the British Insurance Brokers‘ Association and the Association of British Insurers to ensure that wider messages are being heard across the market.
To find out more about how we can assist you see our care insurance webpage or email caredivision@towergate.co.uk. We can also advise on market updates.
Date: November 24, 2022
Category: Care and Medical











